Lip & Tongue-Tie Release
- A tongue-tie is a too thick, tight, or short remnant of tissue from fetal development under the tongue that restricts normal tongue movement and causes a functional issue.
- The symptoms the child has are more important than the appearance. A full assessment of related issues is the key to diagnosing a tongue-tie.
- Having a patient stick the tongue out is the worst test to determine the presence of a tongue-tie. Elevation or having the patient open wide and lift the tongue to the palate is the best quick test for older children, or lifting the tongue on a baby is the best test.
- Elevation or lifting the tongue is the critical movement for the key activities of nursing, swallowing, and speaking.
- A lip-tie is a remnant of tissue that is abnormally tight or thick that causes difficulty lifting the lip as required for nursing, feeding, speech, or for cleaning the teeth. It also can cause a gap in the teeth, and if it is wider than 2mm, it may need to be released and will not likely close on its own (especially if another functional issue is present).
Variable Appearance
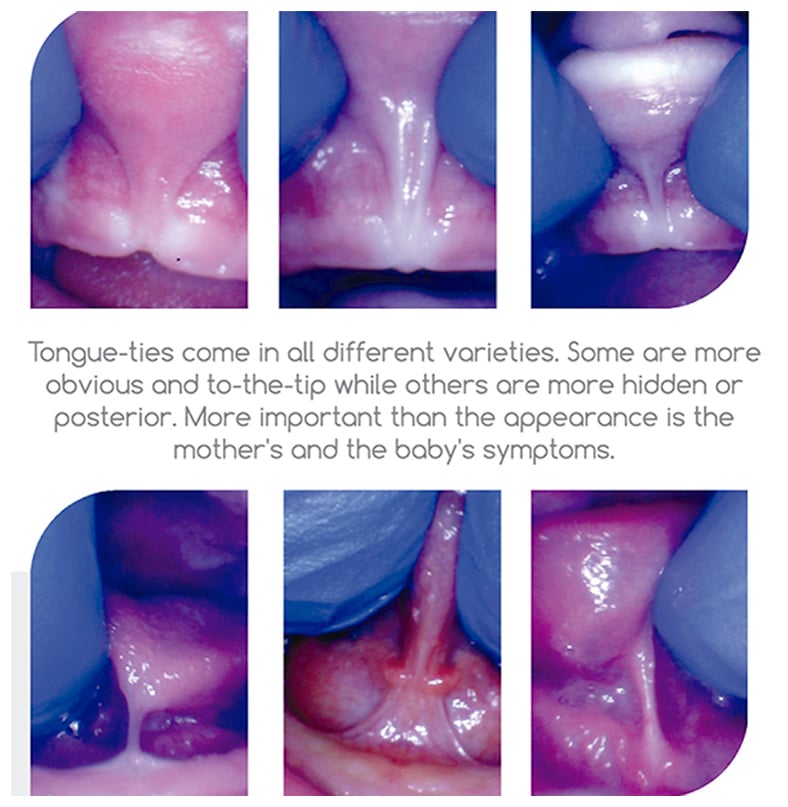
Appearance
Children’s tongue-ties can appear very tight or mildly tight. The symptoms and function are much more important than appearance.
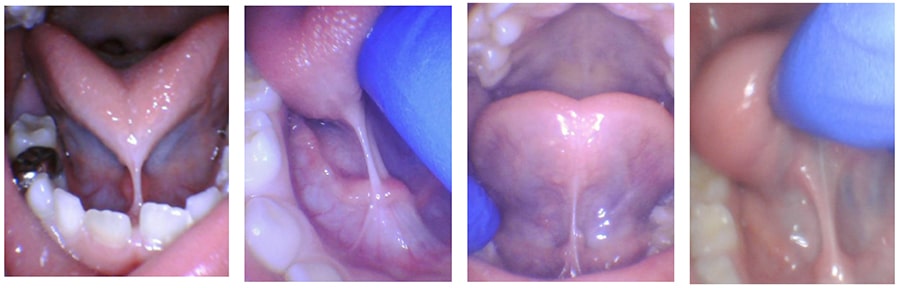
All of these strings under the tongue were causing problems, even ones that don’t appear as significant.
Issues with Tongue-Ties
- Many babies have nursing difficulties that do not resolve.
- Speech issues with R, L, S, TH, speech delay, mumbling, “baby talk”.
- Airway issues because palate and nasal cavity are too narrow.
- Snoring and Sleep Disordered Breathing in kids and adults.
- Feeding issues like difficulty transitioning to solids, swallowing food, slow eating, picky eating, and reflux.
- Dental issues in the future (cavities, gap, narrow palate, braces).
- Mouth breathing leading to ear infections and enlarged tonsils and adenoids is common.
Infant Problems
Infant Symptoms
- Shallow latch / Popping on & off
- Poor or slow weight gain
- Short sleeping and frequent feeding
- Clicking or smacking noises
- Reflux or spitting up often
- Gassy or fussy often
- Snoring, heavy breathing, congestion, choking, gagging
- Milk dribbles out of mouth
- Unable to hold a pacifier
Mother Symptoms
- Painful nursing
- Bleeding, blistered, cracked, creased nipples
- Incomplete breast drainage
- Infected nipples, mastitis, thrush
- Can’t nurse without a nipple shield
Speech Issues
- Difficulty with sounds that require tongue elevation: “S, Z, T, D, L, R”.
- Difficulty with sounds from the posterior aspect: “G, K, N, J”.
- Difficulty with speaking clearly or speaking quickly – “Baby Talk”.
- Stuttering, lisping, or slurring words.
- Speech delay can occur if child has impaired tongue mobility.
Feeding Issues
- Very Picky eating - especially with textures (mashed potatoes, meat, etc.)
- Slow eating – difficulty swallowing leads to slow eating and getting distracted while eating. Possible trouble gaining weight.
- Packing food in the cheeks.
- Spitting out food.
- Swallowing food whole with very little chewing.
- Reflux and constipation.
- Gagging on foods.
- Unable to eat age-appropriate diet.
Sleep Issues
- Sleep disordered breathing /sleep apnea
- Restless sleeping / thrashing around
- Snoring
- Waking up not feeling refreshed
- Waking often during sleep
- Bedwetting
- Tooth grinding
- Mouth breathing
- Sleeping in strange positions
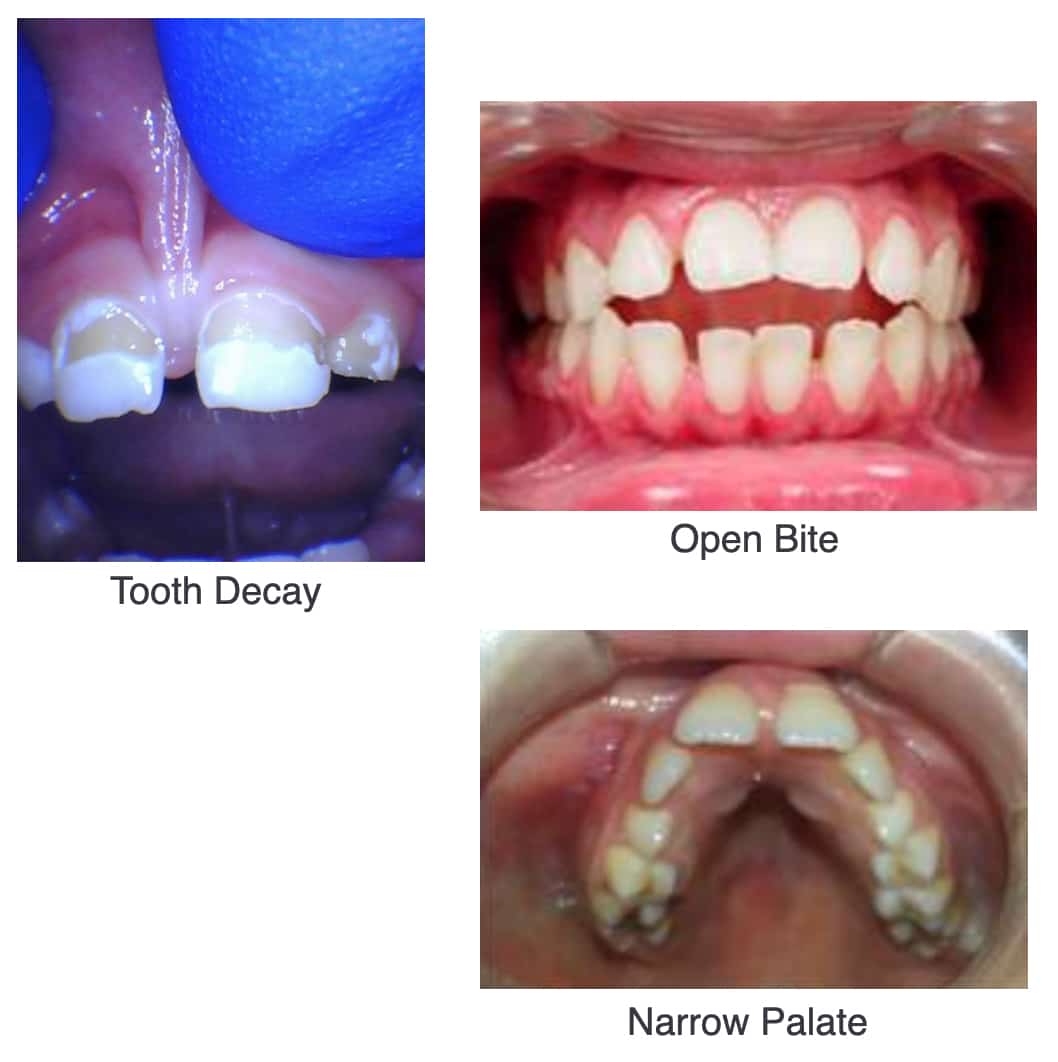
Other Correlated Issues
- ADHD
- Sensory Issues
- Tooth Decay
- Open Bite
- Tooth Grinding
- Tongue Thrust
- High or Narrow Palate
- Frequent ear or sinus infections
- Neck and shoulder tension or pain
- Headaches
- Mouth breathing
Laser Advantages
- Minimal to no bleeding
- Less post-treatment pain than using scissors or a scalpel
- Better visualization during surgery
- Extremely precise
- Virtually no risk of infection
- No need for general anesthesia or sedation
- Very effective
- Excellent healing and less scarring compared to scissors
- We use the highest quality surgical CO2 laser available that vaporizes the tissue instead of burning it like electrocautery or diode lasers.
- Local anesthesia with topical numbing jelly or injected lidocaine are often sufficient to prevent pain during the procedure.
During the Procedure
- We follow all laser safety protocols and use protective eyewear for everyone in the room, including the child.
- We swaddle the infant in a soft wrap to prevent movement that could make the procedure more difficult and ensure the baby’s safety.
- Parents wait in the consult room during the procedure so we can fully focus on your baby and parents watch a short video about post-treatment stretches. We bring your baby back immediately after the procedure is complete to nurse or feed.
- It takes a few minutes to position your baby then approximately 20 seconds for the lip, 10 seconds for the tongue. You baby is back with you in about five minutes. We take before and after photos of the mouth only. These photos do not show your child’s face. They are for medical record and insurance purposes only.
Healing Phase
- We want a baby to nurse or feed right away
- Oral wound healing is rapid
- The scab will turn a white or yellow color after a day or two
- It can look like an infection or pus (but it is not)
- Increased drooling is normal
- Tylenol (any age) and Motrin (if >6mo) for pain – dosed by weight
- A suppository can be used if needed (Feverall).
- Nursing, bottles, nipple shield, pacifiers, sippy cups can be used. Do what you normally would to keep your baby comfortable and eating well. Some parents also work with a lactation consultant or feeding specialist if needed. Try not to change too much else for the baby’s sake right away.
- Soreness typically lasts for 1-3 days.
Post Frenectomy Exercises for Infants
- Done to prevent re-attachment and strengthen the tongue muscles
- 3 times a day for 4 weeks. Plan to coordinate stretches with feedings and diaper changes for babies.
- Keep it as playful as possible with funny noises and faces if baby is older.
- Play with baby’s mouth and tongue when you are not doing exercises to prevent an oral aversion.
- Keep the actual stretching of the wound to just 5-10 seconds for lip, and 5-10 seconds for tongue.
- Use a camping headlight, or have someone hold a flashlight to see the diamond.
- First lift the upper lip high to the nose so the diamond is fully opened, then use a gentle massage on the wound to ensure it does not grow back together.
- For the tongue, come from behind, use one or two fingers to lift the tongue as far up and back as possible to put tension on the wound and ensure the diamond is open.
- Gently massage the wound backward using the same rolling massage motion to encourage the wound to elongate.
Tongue Exercises in Children
- Sample exercises to help with healing are described below and should be performed 2 times a day for 4 weeks or more often if desired.
- Stick tongue out all the way to a point (not flat) by scraping edge of top teeth and pull back and lick top of palate 20x.
- Stick tongue out to the left all the way, right all the way, and touch palate- 10x.
- Push tongue into cheek on R side like a gumball, 10 sec, into L cheek 10 sec.
- Stick tongue out down the chin as far as possible- hold 10 sec.
- Suction the tongue to the palate and open widely and hold for 10 sec.
Reattachment
- Reattachment is simply the natural healing process. Just like a cut on the hand will heal back together, the special cut under the lip or tongue will try to contract and heal together as well. We are trying to “trick” it to stay open.
- Can happen easily if stretches aren’t performed routinely and with enough pressure or tension.
- Make sure to stretch often with sufficient pressure and look at the site with a light. If it looks or feels tight, do a stronger or deeper stretch to open the scab again.
- If symptoms begin to return after they disappeared, then this is the likely reason.
Notes
- Performing exercises is required for best results.
- We make our diagnosis based upon functional issues for the child and related symptoms the child may be experiencing combined with the clinical exam and amount of restriction present under the tongue or lip.
- We do our best to achieve a “full” release.
- We use the latest technology, protocols, and most current methods to provide our patients with the best results and experience possible.
- We educate parents to ensure the child has the best chance of a good outcome, and we often partner with our colleagues like speech therapists, occupational therapists, and myofunctional therapists to facilitate the rehabilitation and help the child achieve normal function.
Follow Up
- We will call later in the afternoon to check on you and your baby/child in case there are any concerns.
- If you have any questions, please call the office.
- Remember, this is a process! It will likely be better in the office, but could get more difficult for a few days, then get progressively better over a few weeks. Expect one better feed a day in infants.